Celiac disease isn’t just a buzzword in the gluten-free community; it’s a serious autoimmune disorder that affects millions worldwide. For those who suffer from it, indulging in bread or pasta can lead to unpleasant and often debilitating symptoms. If you’ve ever felt bloated after eating a slice of pizza or experienced fatigue that seems unexplainable, understanding celiac disease might shed some light on your situation celiac disease treatment.
Navigating life with this condition may feel overwhelming at times, but there are effective treatment options available. From recognizing the signs to implementing dietary changes, knowledge is your best ally in managing and treating celiac disease. Let’s dive deep into what this condition really means and how you can take control of your health journey!
Understanding Celiac Disease: What is it and what causes it?
Celiac disease is an autoimmune disorder that triggers a reaction to gluten, a protein found in wheat, barley, and rye. When someone with celiac consumes gluten, their immune system mistakenly attacks the lining of the small intestine. This damage can lead to malabsorption of nutrients and various gastrointestinal issues.
The exact cause remains unclear. Genetics play a significant role; having relatives with celiac increases your risk. Environmental factors may also contribute. An infection or significant life stressor could potentially act as catalysts for triggering the onset of symptoms.
Interestingly, celiac disease can develop at any age—it’s not limited to childhood. For some individuals, it appears after years of eating gluten without problems. Understanding these fundamental aspects helps demystify this complex condition while shedding light on its serious implications for those affected.
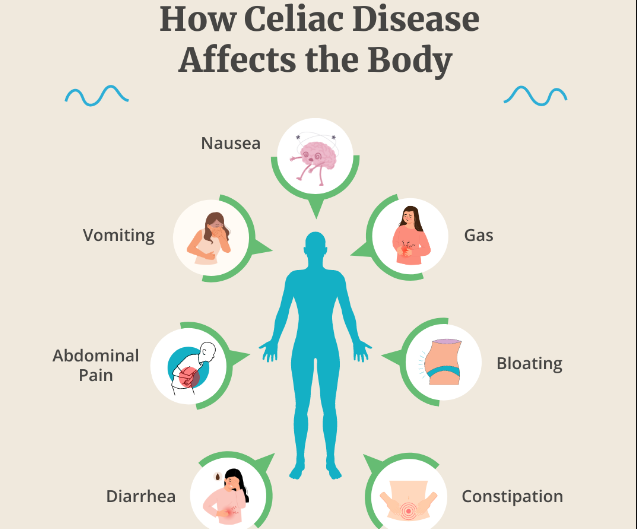
Common Symptoms of Celiac Disease
Celiac disease manifests through a range of symptoms that can vary significantly from person to person. Digestive issues are among the most prevalent, including bloating, diarrhea, and abdominal pain. These discomforts often lead individuals to seek medical advice.
However, celiac disease doesn’t only affect the gut. Many people experience fatigue or unexplained weight loss due to malabsorption of nutrients. Skin reactions like dermatitis herpetiformis also signal an underlying issue with gluten.
Some may encounter neurological symptoms such as headaches or cognitive difficulties known as “brain fog.” Additionally, mood disorders like anxiety and depression have been linked to this autoimmune condition.
Recognizing these diverse symptoms is crucial for early diagnosis and intervention. The complex nature of celiac disease means awareness is key in navigating its challenges effectively.
Diagnosis: How is Celiac Disease diagnosed?
Diagnosing celiac disease can be a multi-step process. It often begins with a thorough review of your medical history and symptom discussion with a healthcare provider.
Blood tests play an essential role in the initial diagnosis. These tests check for antibodies that indicate an immune response to gluten consumption. Elevated levels of specific antibodies typically suggest celiac disease.
If blood tests are positive, a biopsy may follow. This involves taking small tissue samples from the small intestine during an endoscopy. The samples are examined for damage to the villi, which are tiny hair-like structures essential for nutrient absorption.
It’s crucial not to start a gluten-free diet before testing, as this could lead to inaccurate results. Accurate diagnosis is key for effective treatment and management of symptoms associated with celiac disease.
Treatment Options for Celiac Disease
When it comes to celiac disease treatment, the primary approach is strict adherence to a gluten-free diet. This means avoiding any foods containing wheat, barley, and rye. For many, this dietary change can lead to significant improvements in symptoms.
In addition to diet changes, some patients may benefit from nutritional supplements. Since celiac disease often leads to nutrient deficiencies, vitamins and minerals such as iron or calcium might be recommended by healthcare providers.
For those with severe reactions or complications related to celiac disease, corticosteroids could be prescribed for short-term relief of inflammation. However, these are not a long-term solution.
Regular follow-ups with healthcare professionals help track progress and address other health issues that may arise due to the condition. Each person’s journey is unique; therefore, tailored treatments are essential for effective management of celiac disease.
The Gluten-Free Diet: A Key Component of Celiac Disease Treatment
The gluten-free diet is central to effective celiac disease treatment. For those with this condition, consuming gluten—a protein found in wheat, barley, and rye—can trigger severe health issues.
Transitioning to a gluten-free lifestyle may seem daunting at first. It requires careful label reading and meal planning to avoid hidden sources of gluten. Fortunately, many foods are naturally gluten-free. Fruits, vegetables, meats, fish, and dairy are all safe options.
As you begin this journey, consider exploring alternative grains like quinoa or rice. They can provide variety without the discomfort that comes from gluten exposure.
Dining out also presents challenges but isn’t impossible. Many restaurants now offer gluten-free menus or accommodations for individuals with dietary restrictions.
Engagement in support groups can be invaluable too. Connecting with others navigating similar experiences can provide encouragement and practical tips on maintaining a healthy diet while managing celiac disease.
Other Lifestyle Changes to Manage Celiac Disease
Managing celiac disease goes beyond just dietary choices. Incorporating lifestyle changes can significantly enhance your well-being.
Educate yourself about gluten sources. Familiarize yourself with not only food labels but also cosmetics and medications that might contain gluten. Awareness is key.
Consider meal prepping to avoid cross-contamination. Designate specific kitchen tools for gluten-free cooking, like cutting boards and utensils, to keep everything safe.
Physical activity plays an essential role too. Regular exercise can help improve digestion and boost mood, making it easier to cope with the challenges of living with this condition.
Find a community or support group where you can share experiences and tips. Connecting with others who understand what you’re going through creates a sense of belonging and reduces feelings of isolation. Embracing these changes will empower you on your journey toward better health management.
Coping with the Emotional Impact of Celiac Disease
Living with celiac disease can take a toll on emotional well-being. The constant need to avoid gluten may lead to feelings of isolation and frustration. Social situations become challenging, as dining out or attending gatherings often stirs anxiety.
It’s essential to find ways to cope with these emotions. Connecting with others facing similar struggles can provide comfort and understanding. Support groups, both online and in-person, can be valuable resources for sharing experiences.
Practicing mindfulness techniques such as meditation or yoga can help manage stress levels. These practices promote relaxation and encourage a positive mindset.
Additionally, educating family members about celiac disease fosters an environment of support at home. When loved ones understand the condition better, they are more likely to help navigate dietary restrictions together.
Finding joy in cooking new gluten-free recipes also offers an empowering distraction from negative feelings associated with diagnosis or treatment challenges.
Support and Resources for Those Living with Celiac Disease
Living with celiac disease can feel isolating, but you’re not alone. Numerous organizations provide valuable support and resources tailored for those navigating this condition.
The Celiac Disease Foundation is a great starting point. They offer educational materials, gluten-free recipes, and community events that foster connection among individuals affected by celiac disease.
Online forums and social media groups create spaces where you can share experiences or ask questions. Engaging with others who understand your journey can be incredibly uplifting.
Local support groups also exist in many areas. These gatherings allow individuals to meet face-to-face, discuss challenges, and swap tips on managing daily life while adhering to a strict gluten-free diet.
Additionally, healthcare professionals specializing in nutrition can guide dietary choices. Resources like certified dietitians play an essential role in helping manage the intricacies of living without gluten effectively.
Conclusion: Finding
Finding the right approach to celiac disease treatment can be a journey filled with learning and adaptation. Understanding the intricacies of this autoimmune disorder is crucial. Each person’s experience may vary, but knowledge fosters empowerment.
A gluten-free diet serves as the cornerstone of effective management for many individuals. However, it isn’t just about what you eat; it’s also about embracing lifestyle changes that enhance your overall well-being. Emotional support plays a significant role too, as navigating dietary restrictions can sometimes feel isolating.
Connecting with communities or seeking professional guidance provides invaluable resources on this path. With patience and determination, managing celiac disease becomes achievable—allowing individuals to lead fulfilling lives despite challenges.
Finding balance in daily routines and maintaining awareness are key steps toward thriving with celiac disease. As more people share their experiences, we collectively build an understanding that promotes better health outcomes for everyone affected by this condition.